[Author’s Note: I thought this was published last week. I guess the holidays took more out of me than I thought…]
Out of the total Medicare budget, something on the order of $ 30 billion is allocated to dialysis (6% of total Medicare costs). Over the years, Medicare has increased the lag time with which they cover the costs of dialysis from 12 to 33 months (due to industry lobbying); once covered by the ESRD program, Medicare pays 80% of the costs, with Medicaid or existing insurance covering the remaining 20%. [Medicare reimburses at a lower rate than commercial insurance, which is why
industry lobbied for a longer lag phase.]
Starting next year, the method by which providers will be paid for this treatment will begin to change. All dialysis costs will be bundled [prospective payment system (PPS)] for out-patients (acute care, for a specific episode of treatment due to accident, heart failure, etc. is not part of the ESRD program)- this means treatment costs, supplies, required lab tests, and some drugs. Reimbursement will be tied to quality achievement outcomes (initially, three specific measures).
A four-year transition period is contemplated, where a blend of the old and the new reimbursement process will be possible. (The larger firms have opted for this blended rate, as opposed to fully engaging in the new PPS.) The new process is based upon a payment of $ 229.63 for each treatment, but that is adjusted for case mix, pediatric patients, self-dialysis training, among other issues. There will be a 2% rate reduction if quality of care does not meet
standards.
A primary change under the PPS is that anemia management (which has been heretofore handled via administration of erythropoiesis stimulating agents (ESA) (e.g., Epogen)  is a primary the quality measures (50% of the score, maximum overall score is 30). Hemoglobin numbers must be maintained between 10 and 12 g/dL. This will radically affect the usage rates of ESA; it also has been
one of the more lucrative methods to obtain additional reimbursement. The other measure is the adequacy of dialysis (as manifested by the urea reduction ratio; 65% is the target minimum. (Note: the calculations are ONLY for Medicare patients, not ALL patients.)
Another factor helping patients is that
reimbursement will be per treatment, as opposed to per month or week; this affords patients flexibility as to where they can undergo treatment (such as vacations, etc.).
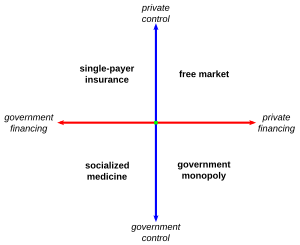
While the PPS as proposed by Medicare only refers to dialysis, one can begin to postulate how the new health care program will be implemented for all medical disciplines. (Note: Medicare is about 19% of the total US health care expenditures.) As we used to say when we were providing dialysis therapy, we had one customer with thousands of intermediaries (Medicare paid for all dialysis, there were 3500 dialysis clinics who purchased our wares. This is the lower left quadrant in the diagram.) The dialysis quality measures are based upon FDA guidelines and published evidence-based medicine. One would expect the new health care guidelines use outcome based results to manage the practice of medicine. (The health care legislation passed this year moves the system from mostly in the upper right quadrant [Medicaid and Medicare are in the upper left] to mostly in the lower right quadrant.)  And, like the
dialysis measures, some of the parametric choices may actually count twice (e.g., the hemoglobin measurements are bounded by a maximum and minimum value).
[prepared 14 September]